
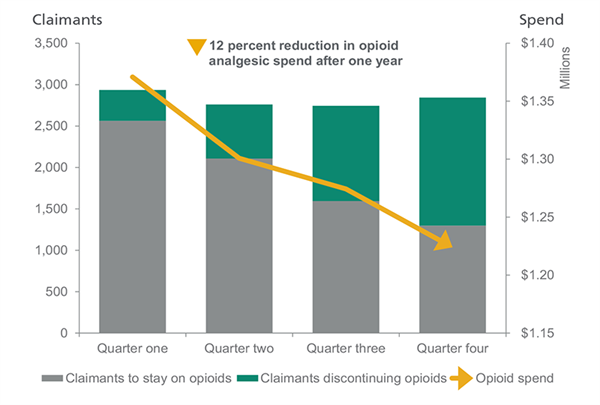
Learn how clinical alerts driven by predictive analytics helped TPA executive Lynda cut opioid spend 12% over the previous year and provide adjusters and case managers with tools to improve outcomes for clients and claimants.
Clinical alerts help manage costs and improve outcomes by identifying potential medication-use risks and recommending alternatives that save money and enhance claimants’ progress.
Meet Lynda

Lynda is the Vice President of Claims for a TPA. She is responsible for ensuring all of her adjusters manage their claims efficiently and effectively, thereby securing the largest possible savings for their clients. When the time came for her company to select a new Pharmacy Benefits Manager (PBM) provider, one of the main requirements was that the PBM have a clear and simple way to help their adjusters manage claims more effectively. Lynda’s company selected Optum because of the large number of features available that would ensure better clinical oversight over their claims.
Optum clinical services
The enterprise-wide suite of clinical services provided by Optum works across all phases of the claim lifecycle to promote claimant health and wellness, reduce the risk of poor health outcomes and contain costs. Their program effectively leverages data intelligence to help manage a claim from injury to settlement. Through extensive data analysis and predictive modeling capabilities, Optum proactively identifies and addresses potential risks that can inflate costs and delay a claimant’s progress. Levels of care are designed to clinically monitor and assess proper utilization and appropriateness of therapy based on the progression point of the claim from prospective controls, to concurrent interventions and retrospective services.
These specialty services are comprehensive solutions that integrate the capabilities of specific interventions to address complex issues including:
- Predictive analytics
- Population risk assessment
Collaborative effort
As part of the transition to Optum, Lynda met the Optum team to determine edits, formularies, and plan specifics that would be put into place for her company’s claims. While the standard clinical guidelines for treatment, such as Official Disability Guidelines (ODG) and state-specific treatments would be uploaded into the system, Optum could also accommodate Lynda’s company-specific guidelines. This customization helped ensure her claims were managed the way she and her company wanted them.
The right expectations
Once implementation was complete, Lynda’s adjusters began receiving Clinical Alerts for their claims. These notifications communicated when claimants varied from their treatment plan, such as taking opioids for longer than 90 days, or going over the 120 MED per day guidelines. Adjusters could then review and elect the appropriate actions for the claim; whether they be a medication review, or sending the claimant for drug testing.
Optum delivers savings
After partnering with Optum for a year, Lynda found that of all of the Clinical Alerts involving opioids, 65% of claimants could either have their opioids discontinued immediately, or be weaned off over a period of time. That allowed her to decrease their overall spend on opioids 12% over the previous year. A huge win for the company.
Follow up
By partnering with Optum, Lynda was able to provide her adjusters and case managers with efficient tools to ensure the best care for their claimants’ health, and their clients’ bottom lines. A win-win for everyone.