
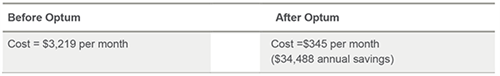
Learn how a Medication Review saved one company more than 89%, almost $35,000 annually, on one claimant’s medication expenses and how Jenny’s pain improved significantly after a change in her medication regimen.
A Medication Review evaluates a claimant’s medication therapy to identify medication-related concerns and develop a plan to resolve them ─ resulting in improved claimant outcomes and ensuring that dollars are not spent on inappropriate treatment.
Meet Jenny

“I was hurt in one of the oddest ways possible. My company requires a biometric screening as part of its insurance plan, and during a simple blood draw procedure, the needle wiggled a bit and there was an immediate shooting pain up and down my arm. My right arm was always in pain, and my right thumb was usually numb. It had a huge impact on my life, not only could I not work, since I am right-handed, but it also prevented me from doing the other things I loved, like working out.”
Jenny’s doctor diagnosed her with complex regional pain syndrome (CRPS) type 2, and prescribed the following medications:
| Medication name | Directions | Prescribed strength |
|---|---|---|
| Tapentadol Tab | One tablet twice a day | 50 mg |
| Tramadol HCI Tab SR 24 hr | One tablet twice a day | 100 mg |
| Lidocaine Patch | One patch daily, up to three at one time | 5% |
| Gabapentin Cap | One capsule twice a day | >300 mg |
| Lamotrigine Tab | Three tablets per day |
25 mg |
| Nortriptyline HCI Cap | One capsule once a day | 10 mg |
| Compound (Baclofen – Cyclobenzaprine – Diclofenac – Ketoprofen – Tetracaine) |
Apply four times daily | |
Predicting potential problems
Since Jenny’s case was being processed through the Optum pharmacy benefit management (PBM) system, her plan of care was automatically routed through their Predictive Analytics, which determined that she could potentially have medication issues. A clinical review occurred where it was determined that Jenny needed a Medication Review, which provided an in-depth review of all of her medication therapy.
The comprehensive Medication Review by Optum provides an individualized evaluation of a claimant’s current medication therapy by a Clinical Pharmacist to identify any medication-related concerns and develop an action plan for problem resolution. Intended for high-risk, actively managed cases not in the process of settling, the Medication Review helps ensure the claimant is on the right medication regimen for optimal long-term outcomes—so that dollars are not spent on unnecessary or inappropriate treatment.
The Medication Review determined that Jenny was on a high-cost compound medication that could be discontinued due to lesser cost alternatives. There were also concerns of duplicate therapy and dosage appropriateness. A Peer-to-Peer Outreach was ordered so that Jenny’s medications could be reviewed by another experienced doctor and then discussed with her treating doctor. A Peer-to-Peer Outreach increases the likelihood that the recommended medication changes will be implemented by the prescribing doctor and promotes safer, more effective care for the claimant.
Changes made
Following the Peer-to-Peer Outreach, Jenny’s doctor agreed to discontinue the compound medication and reduce the frequency of the short-acting opioid analgesic to just once a day, as needed. He also agreed that the dosage of her nerve pain medications should be reduced to half.
Savings calculation
Follow-up
“I am now on different medications and I am beginning to see some improvement. Instead of a pain level of 7 or more all the time, I am now down to a 3 or 4 most days. I started back to work, although limited for now. I even went to a yoga class the other day. I know I have a long road ahead of me, but now I have hope that my life can get back to normal,” says Jenny.
